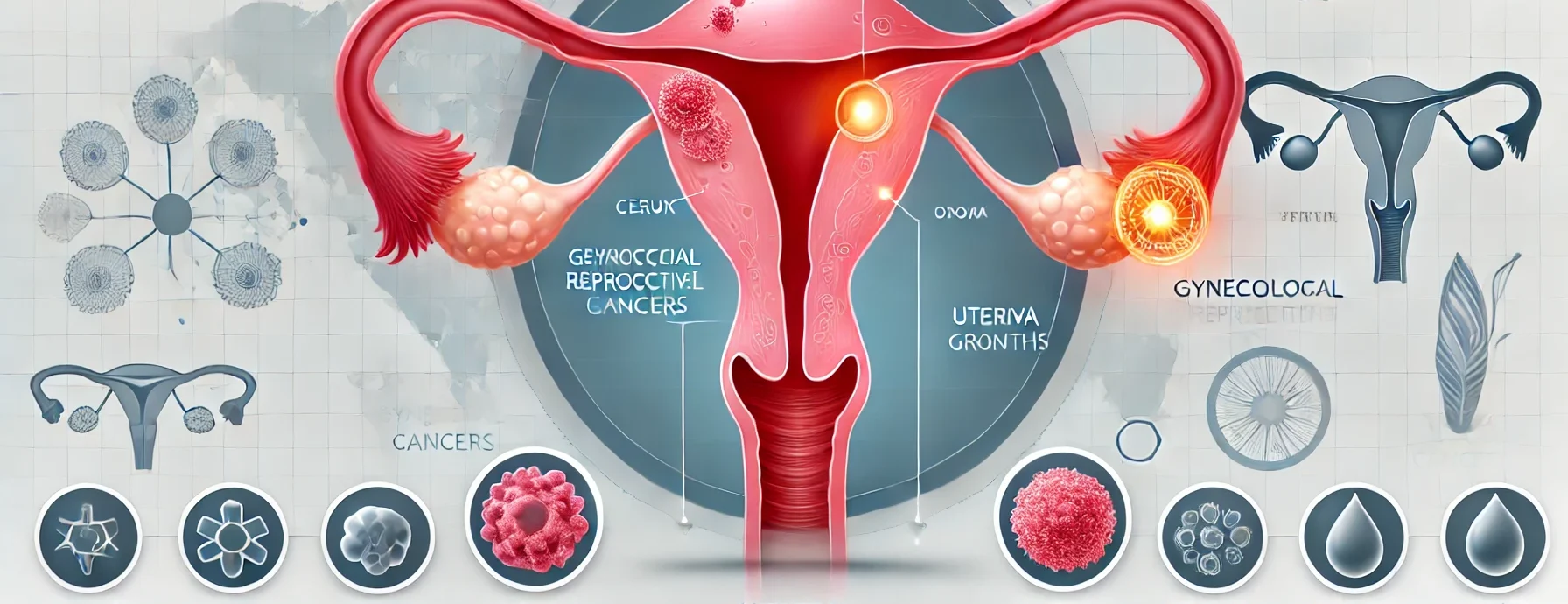
What is Gynecological Cancer?
Gynecological cancer refers to any cancer that starts in a woman’s reproductive organs. The five primary types include:
- Cervical Cancer: Begins in the cervix, often linked to human papillomavirus (HPV).
- Ovarian Cancer: Affects the ovaries, often detected at a late stage.
- Uterine (Endometrial) Cancer: Starts in the lining of the uterus, common in postmenopausal women.
- Vaginal Cancer: A rare cancer that develops in the vaginal tissues.
- Vulvar Cancer: Affects the outer part of the female genitalia.
Each type of gynecological cancer has distinct symptoms, risk factors, and treatment approaches. Early detection is crucial for effective treatment.
Symptoms of Gynecological Cancer
The symptoms vary depending on the type of cancer but commonly include:
- Abnormal vaginal bleeding (after menopause, between periods, or post-intercourse)
- Unusual vaginal discharge (bloody, watery, or foul-smelling)
- Pelvic pain or pressure
- Pain during intercourse
- Frequent or painful urination
- Changes in bowel habits, such as constipation or diarrhea
- Persistent bloating or swelling in the abdomen
- Unexplained weight loss or gain
- Persistent fatigue
If you experience any of these symptoms for more than a few weeks, consult a doctor immediately.
Causes and Risk Factors
While the exact cause of gynecological cancers varies, several risk factors contribute to their development:
- HPV Infection: A leading cause of cervical and vaginal cancers
- Age: Risk increases with age, especially post-menopause
- Family History: A genetic predisposition can increase the risk
- Obesity: Linked to an increased risk of endometrial and ovarian cancers
- Smoking: Raises the risk of cervical, vulvar, and vaginal cancers
- Hormonal Imbalances: Prolonged estrogen exposure can lead to uterine cancer
- Weakened Immune System: Increases vulnerability to infections that may lead to cancer
Screening and Diagnosis
Early detection of gynecological cancer significantly improves survival rates. Common screening and diagnostic procedures include:
Screening Methods:
- Pap Smear: Detects precancerous or cancerous cells in the cervix
- HPV Test: Identifies high-risk HPV strains that cause cervical cancer
- Pelvic Exam: A routine examination to check for abnormalities
- Transvaginal Ultrasound: Provides detailed images of the reproductive organs
Diagnosis Methods:
- Biopsy: A sample of tissue is taken for microscopic examination
- Blood Tests (CA-125 for Ovarian Cancer): Measures cancer-related proteins
- Imaging Tests (MRI, CT scans, PET scans): Detects tumor size and spread
- Colposcopy: A magnified examination of the cervix for abnormal cells
Treatment Options for Gynecological Cancer
Treatment depends on the type, stage, and location of the cancer. The main treatment options include:
1. Surgery
- Hysterectomy: Removal of the uterus (common for uterine cancer)
- Oophorectomy: Removal of ovaries (for ovarian cancer)
- Lymph Node Removal: Determines if cancer has spread
2. Radiation Therapy
- Uses high-energy rays to destroy cancer cells
- Commonly used for cervical, vaginal, and vulvar cancers
3. Chemotherapy
- Uses drugs to kill cancer cells or stop their growth
- Given orally or intravenously (IV)
4. Targeted Therapy
- Uses drugs that specifically attack cancer cells while sparing normal cells
- Often used for advanced ovarian cancer
5. Immunotherapy
- Boosts the immune system to fight cancer
- Effective for certain cases of cervical cancer
When to Consult a Specialist
You should consult a gynecological oncologist if:
- You experience persistent symptoms like abnormal bleeding, pelvic pain, or unusual discharge
- Your Pap smear results are abnormal
- You have a family history of ovarian or uterine cancer
- You receive a diagnosis requiring specialized cancer treatment
Early consultation with a specialist improves treatment success and survival rates.
5 Frequently Asked Questions (FAQs)
1. Can gynecological cancer be prevented?
While not all cases are preventable, you can reduce your risk by getting the HPV vaccine, maintaining a healthy weight, quitting smoking, and attending regular screenings.
2. What are the early signs of gynecological cancer?
The most common early signs include abnormal bleeding, pelvic pain, bloating, and unusual discharge. Any persistent symptoms should be checked by a doctor.
3. Is gynecological cancer hereditary?
Some types, like ovarian and uterine cancer, can be hereditary. Genetic testing can help assess your risk if you have a family history.
4. What is the survival rate of gynecological cancer?
Survival rates depend on the type and stage of cancer. When detected early, the survival rate is significantly higher.
5. How often should I get screened?
Regular Pap smears are recommended every three years for women aged 21-65, or every five years if combined with an HPV test. Other screenings depend on your risk factors.