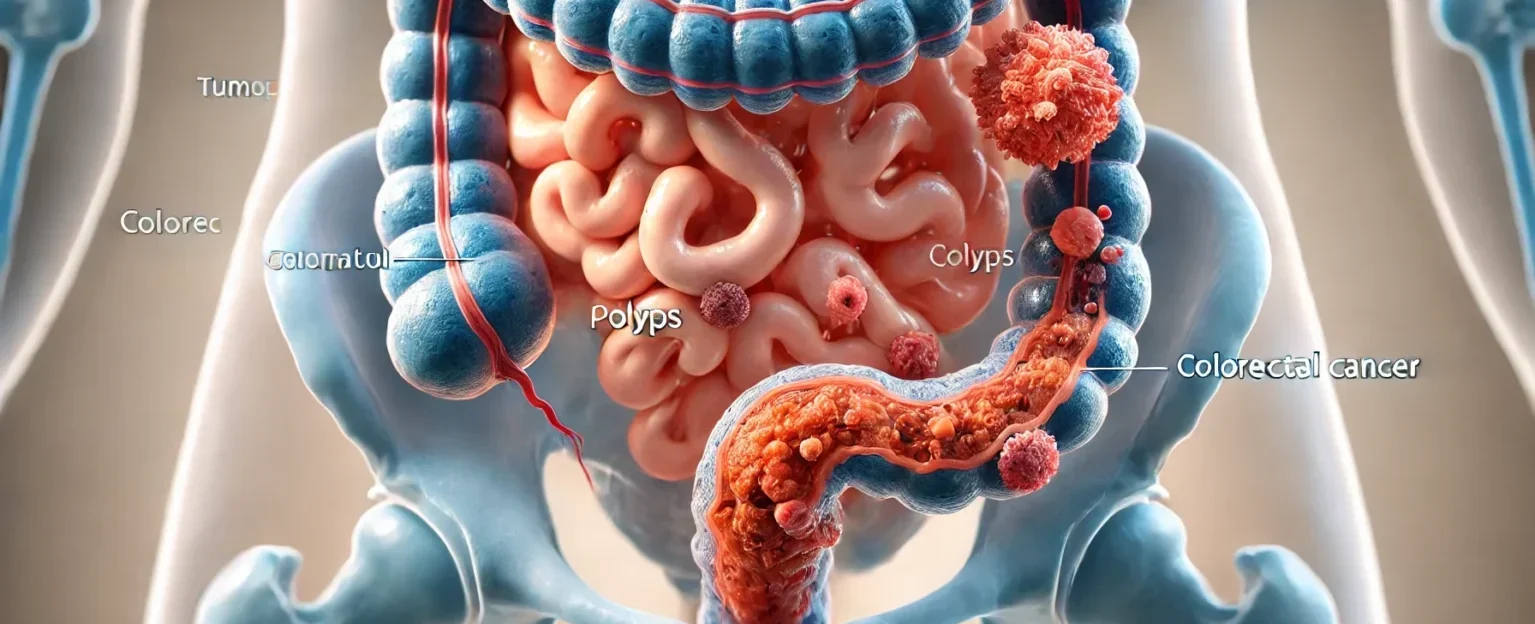
Colorectal cancer is a serious and potentially life-threatening disease that originates in the colon or rectum. This form of cancer often begins as small, benign growths known as polyps. While these polyps may not initially pose a risk, over time, some can develop into cancerous tumors if left untreated. The most effective way to prevent colorectal cancer from advancing to a more severe stage is through early detection and medical intervention. When diagnosed in its early stages, colorectal cancer is highly treatable, significantly increasing a patient’s chance of recovery and survival.
Colorectal cancer is one of the most prevalent cancers worldwide, affecting millions of individuals each year. Despite its widespread occurrence, colorectal cancer remains largely preventable through regular screenings, lifestyle modifications, and proper medical care. Understanding the risk factors, symptoms, causes, and available treatment options can empower individuals to take proactive steps in safeguarding their health and minimizing the risk of developing colorectal cancer.
What Causes Colorectal Cancer?
While the exact cause of colorectal cancer varies among individuals, several key risk factors have been identified as contributing to the development of this disease:
Genetic Predisposition
A family history of colorectal cancer significantly increases an individual’s likelihood of developing the disease. Genetic mutations inherited from family members can predispose individuals to the formation of cancerous cells in the colon or rectum. Specific genetic syndromes, such as Lynch syndrome and familial adenomatous polyposis (FAP), have been linked to an increased risk of colorectal cancer.
Dietary Factors
Diet plays a crucial role in the development of colorectal cancer. A diet that is low in fiber and high in fat, particularly saturated fats and processed foods, has been associated with an increased risk. The consumption of red and processed meats, as well as diets high in sugar and refined carbohydrates, may contribute to the formation of precancerous polyps in the colon. Conversely, a diet rich in fruits, vegetables, whole grains, and lean proteins can help reduce the risk.
Age
Advancing age is a significant risk factor for colorectal cancer. The majority of cases occur in individuals over the age of 50. However, in recent years, an increasing number of younger individuals have been diagnosed with colorectal cancer, highlighting the importance of early screening and preventive measures.
Inflammatory Bowel Diseases
Chronic inflammatory conditions such as Crohn’s disease and ulcerative colitis can lead to prolonged inflammation of the colon, increasing the likelihood of abnormal cell growth and the eventual development of colorectal cancer.
Lifestyle Factors
Several lifestyle choices have been linked to an increased risk of colorectal cancer, including:
- Smoking: Long-term tobacco use has been associated with the development of various cancers, including colorectal cancer.
- Excessive Alcohol Consumption: Heavy alcohol intake can contribute to inflammation and cellular changes that may increase cancer risk.
- Obesity: Being overweight or obese has been identified as a risk factor for colorectal cancer, particularly in men.
- Sedentary Lifestyle: Lack of physical activity can contribute to weight gain and metabolic imbalances that may elevate cancer risk. Engaging in regular exercise can help mitigate these risks.
Recognizing the Symptoms of Colorectal Cancer
In its early stages, colorectal cancer may not present noticeable symptoms, making regular screenings crucial for early detection. However, when symptoms do occur, they may include:
- Persistent Changes in Bowel Habits: Chronic constipation, diarrhea, or alterations in stool consistency that persist over time may be warning signs.
- Blood in Stool or Rectal Bleeding: The presence of blood in the stool, whether bright red or dark and tarry, should never be ignored and requires immediate medical evaluation.
- Unexplained Weight Loss: Sudden weight loss without any changes in diet or physical activity may be indicative of an underlying health issue.
- Abdominal Pain or Cramping: Ongoing discomfort, bloating, or cramping in the abdominal area should be assessed by a healthcare professional.
- Weakness or Fatigue: Feeling persistently weak or fatigued may be caused by anemia due to internal bleeding associated with colorectal cancer.
If you experience any of these symptoms for an extended period, seeking prompt medical attention is essential to determine the underlying cause and initiate appropriate treatment if necessary.
The Importance of Screening for Colorectal Cancer
Early detection plays a crucial role in improving colorectal cancer survival rates. Various screening methods are available to detect precancerous polyps or early-stage cancer before symptoms develop. These include:
- Colonoscopy: A comprehensive examination of the colon using a flexible tube equipped with a camera to identify and remove polyps before they become cancerous.
- Stool-Based Tests: These non-invasive tests check for hidden blood or genetic markers linked to colorectal cancer.
- CT Colonography: Also known as a virtual colonoscopy, this imaging test provides a detailed view of the colon to identify any abnormalities.
Medical guidelines recommend that individuals begin colorectal cancer screenings at age 45, or earlier if they have a family history or other risk factors. Routine screenings can significantly reduce the likelihood of advanced-stage cancer development.
Diagnosis Process for Colorectal Cancer
If an abnormality is detected during screening, further diagnostic tests will be conducted to confirm the presence and stage of colorectal cancer. These tests may include:
- Biopsy: A small tissue sample is taken from the affected area for microscopic examination.
- Imaging Tests: CT scans, MRIs, and PET scans help determine whether cancer has spread beyond the colon.
Following a confirmed diagnosis, a personalized treatment plan will be developed based on the stage of cancer and the patient’s overall health condition.
Treatment Options for Colorectal Cancer
The treatment approach for colorectal cancer depends on its stage at diagnosis:
Stage I
- Surgical removal of the tumor is often sufficient, and the prognosis is generally very favorable.
Stage II
- Surgery remains the primary treatment, but chemotherapy may be recommended in cases with high-risk features.
Stage III
- A combination of surgery, chemotherapy, and radiation therapy is typically used to prevent the cancer from spreading further.
Stage IV
- In advanced cases, treatment focuses on palliative care, targeted therapy, immunotherapy, and chemotherapy to enhance quality of life and prolong survival.
When to See a Specialist?
If you notice any of the following warning signs, consult a colorectal specialist immediately:
- Persistent changes in bowel habits
- Blood in stool
- Unexplained weight loss
- Chronic fatigue or weakness
Ignoring these symptoms can delay diagnosis and allow cancer to progress to an advanced stage. Early intervention is critical for successful treatment outcomes.
Frequently Asked Questions (FAQs)
- Can colorectal cancer be prevented?
- Yes! Maintaining a healthy diet, engaging in regular physical activity, and undergoing routine screenings can significantly lower the risk of colorectal cancer.
- What is the survival rate for colorectal cancer?
- Survival rates depend on how early the cancer is detected. The five-year survival rate for localized colorectal cancer exceeds 90%, whereas late-stage diagnoses have lower survival rates.
- At what age should I start screenings?
- Screenings are recommended starting at age 45, though individuals with a family history or additional risk factors should consider starting earlier.